Frequently Asked Questions About the Medicare Prescription Payment Plan
If you believe that any delay in filling the prescription(s) due to the 24 hours timeframe required to process the request to opt in may seriously jeopardize your life, health, or ability to regain maximum function; and you requests retroactive election within 72 hours of the date and time the urgent prescriptions were filled, we can retroactively enroll you in the program effective the date of your request. You will need to pay for the out-of-pocket costs for those prescriptions at the pharmacy, and we will reimburse you for your costs. You will then receive a monthly bill for those prescription costs that will be spread out over the calendar year.
If you determine that the Medicare Prescription Payment Plan isn’t benefitting you after you’ve enrolled, you may opt out of the program at any time. If you are currently enrolled in the payment plan and do not wish to continue your enrollment for the next plan year, you can opt out before the next plan year. To opt out, go to https://www.express-scripts.com/mppp or call 1-866-845-1803 (TTY 1-800-716-3231) 24 hours a day, seven days a week. If you opt out of the program but have already filled prescriptions at the pharmacy after opting-in, you will still be responsible for the monthly bill for those prescription costs. After you opt out, you’ll pay the pharmacy directly for new out-of-pocket prescription costs.
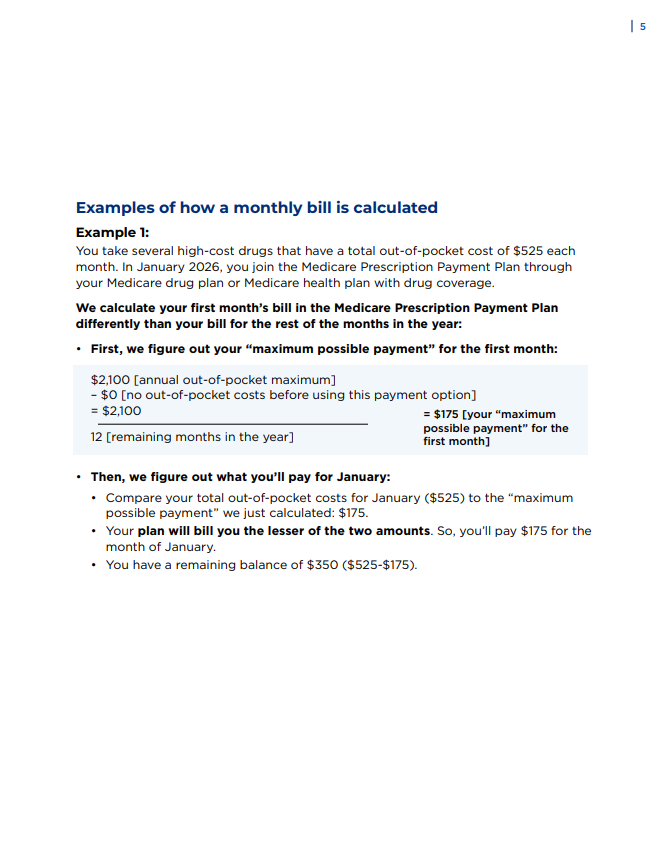
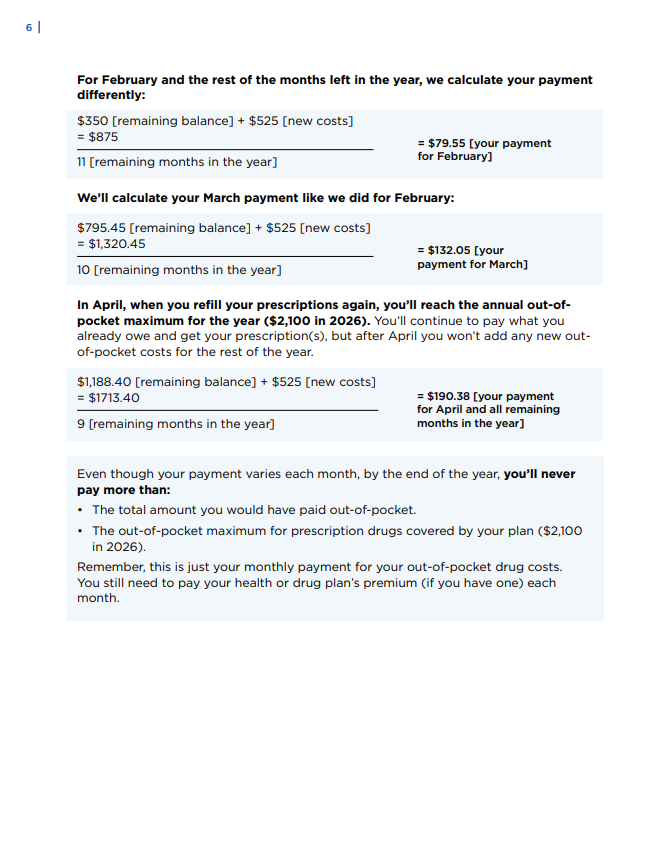
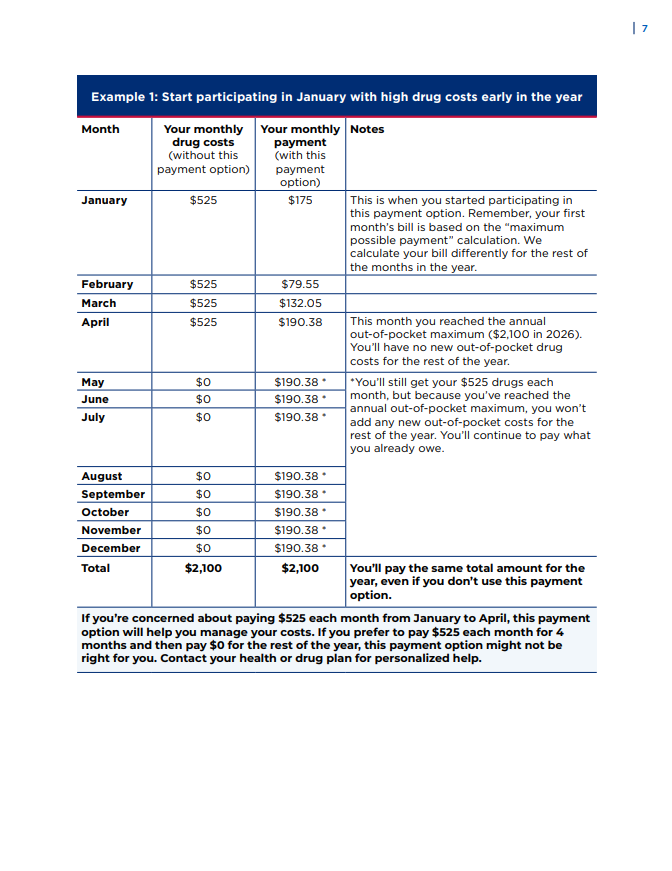
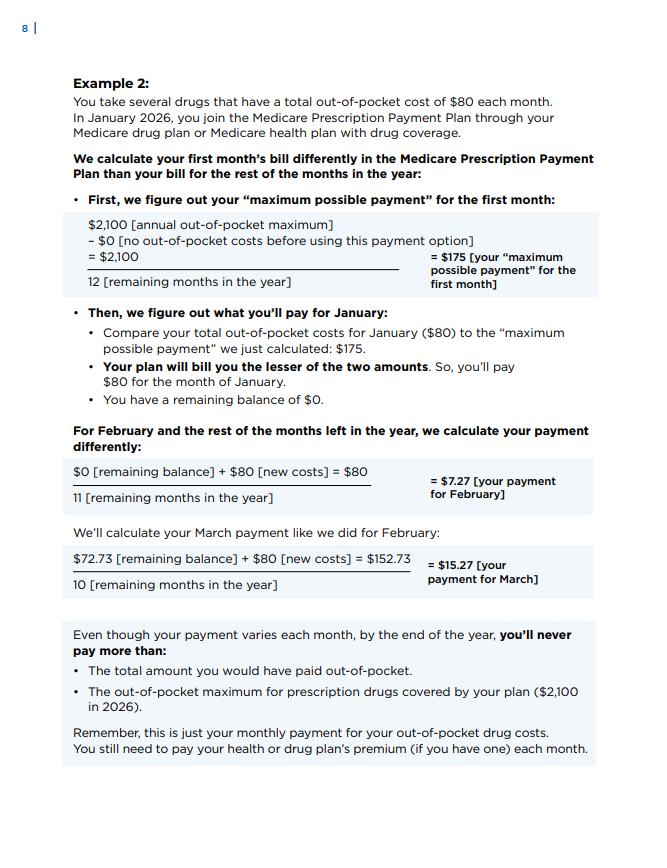
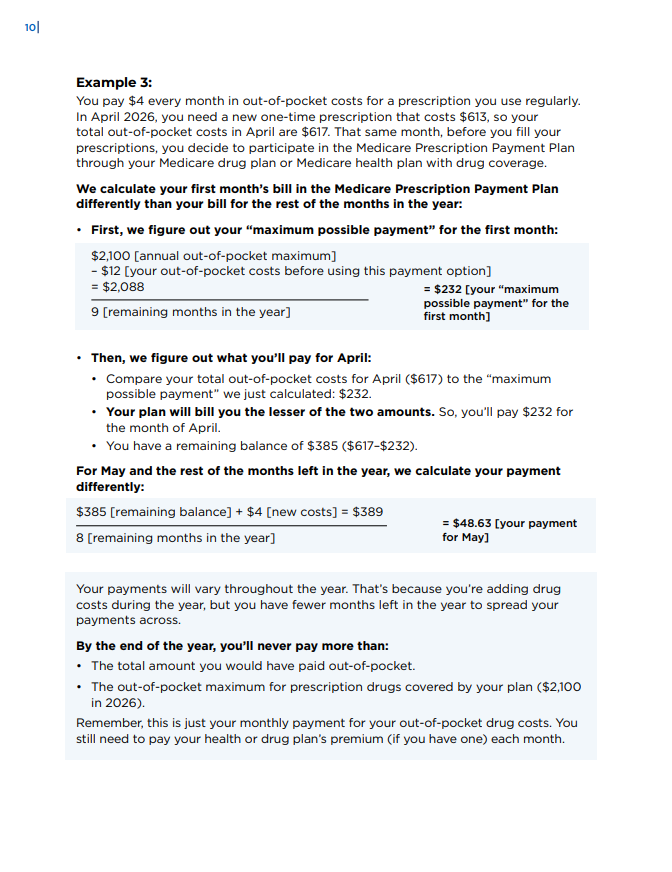
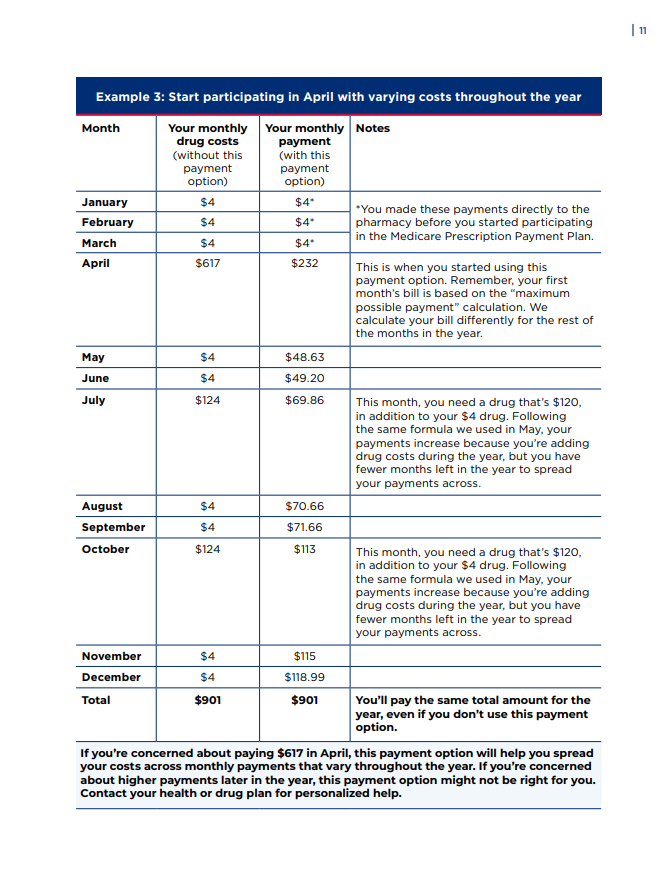
The program is available for all Network Health Medicare Advantage members with Part D prescription drug coverage, but it may not be beneficial for you to opt in. Generally, if you have a single prescription that costs $600 or more per fill or you will pay $2,100 out of pocket for your Part D prescription drugs during the plan year, you may benefit from this program. For the 2026 plan year, $2,100 is the most any member with Medicare Part D prescription drug coverage will pay out-of-pocket for Part D prescription drugs. If you have questions on whether it will be beneficial for you to opt in, call us and we can go over that with you. We can be reached at 1-866-845-1803 (TTY 1-800-716-3231) 24 hours a day, seven days a week.
This program may not be the best choice for you if the following apply.
- Your yearly drug costs are low.
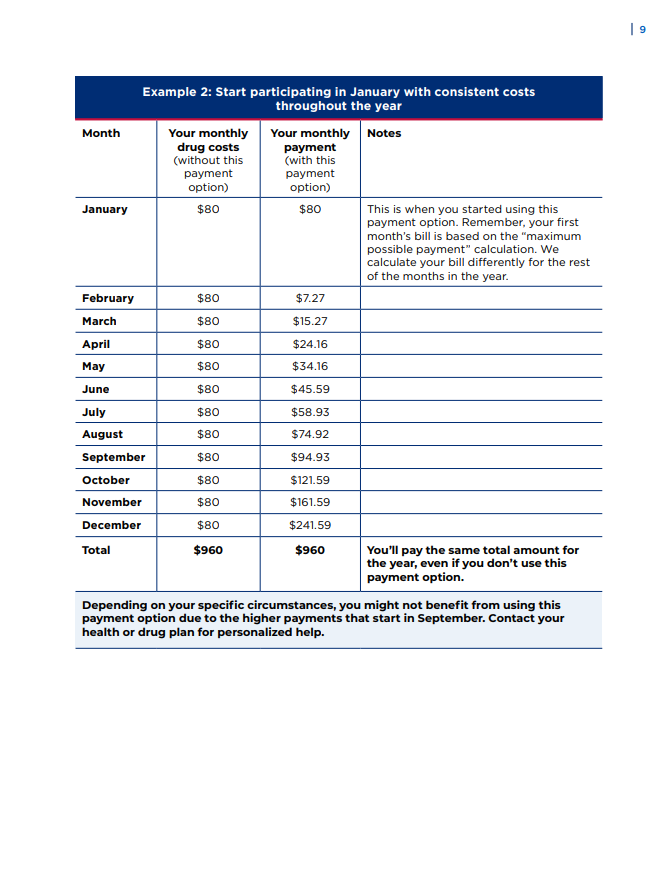
- Your drug costs are the same each month.
- You’re considering signing up for the payment option late in the calendar year (after September).
- You don’t want to change how you pay for your drugs.
- You get or are eligible for Extra Help from Medicare.
- You get or are eligible for a Medicare Savings Program.
- You get help paying for your drugs from other organizations, like a State Pharmaceutical Assistance Program (SPAP), like Wisconsin Senior Care, a coupon program, or other health coverage.
We will send you a reminder if you miss a payment. If you don’t pay your bill by the date listed in that reminder, you’ll be removed from the Medicare Prescription Payment Plan. You’re required to pay the amount you owe, but you won’t pay any interest or fees, even if your payment is late. You can choose to pay that amount all at once or be billed monthly. If you’re removed from the Medicare Prescription Payment Plan, you’ll still be enrolled in your Medicare health or drug plan.
Always pay your health or drug plan monthly premium first (if you have one), so you don’t lose your drug coverage.
If you think there is a mistake with your bill, call us and we’ll go over your bill with you. We can be reached at 1-866-845-1803 (TTY 1-800-716-3231) 24 hours a day, seven days a week. If you want to file a grievance about a mistake with your bill, you can submit your grievance to us by calling 800-378-5234 (TTY 800-947-3529) Monday through Friday, 8 a.m. to 8 p.m. CST. Otherwise, you can submit your grievance in writing to the following address.
Network Health Medicare Advantage Plans
Attn: Appeals and Grievances
P.O. Box 120
1570 Midway Place
Menasha, WI 54942
If you have limited income and resources, find out if you’re eligible for one of these programs:
- Extra Help: A Medicare program that helps pay your Medicare drug costs. Visit ssa.gov/medicare/part-d-extra-help to find out if you qualify and apply. You can also apply with your State Medical Assistance (Medicaid) office. Visit medicare.gov/basics/costs/help/medicaid to learn more.
- Medicare Savings Programs: State-run programs that might help pay some or all
- Wisconsin Senior Care: A program for older adults to help pay for prescription drugs and vaccines. Visit dhs.wisconsin.gov/seniorcare/index.htm to learn more.